Eczema vs Psoriasis: An In-Depth Overview
Welcome to our comprehensive overview of eczema and psoriasis. In this section, we will focus on eczema, exploring its causes, triggers, and various treatment options. Eczema is a chronic skin condition that affects millions of people worldwide, causing discomfort and frustration. By understanding the root causes and effective management techniques, individuals can take control of their eczema and lead a fulfilling life.
Causes of Eczema:
Eczema can be triggered by various factors, including genetic predisposition, allergies, and environmental factors. Those with a family history of asthma, hay fever, or eczema are more likely to develop the condition. Additionally, exposure to irritants and allergens like harsh soaps, detergents, certain fabrics, and pet dander can exacerbate symptoms.
Managing Eczema:
While there is no permanent cure for eczema, there are numerous strategies for managing its symptoms and reducing flare-ups. It’s essential to establish a consistent skincare routine that includes gentle cleansing, moisturizing, and the use of specialized eczema-friendly products. Avoiding triggers, such as stress, certain foods, and extreme temperatures, can also help prevent flare-ups. In severe cases, dermatologists may recommend prescription medications or therapies tailored to the individual’s needs.
“Eczema can be triggered by various factors, including genetic predisposition, allergies, and environmental factors.” – Dermatology Expert
The Importance of Moisturizing:
Keeping the skin properly moisturized is crucial for managing eczema. Regularly applying a thick, fragrance-free moisturizer can help soothe dryness and prevent skin irritation. Look for products that contain ingredients like ceramides, which can help restore and strengthen the skin’s barrier function.
Choosing the Right Treatment:
When it comes to treating eczema, there is no one-size-fits-all approach. The ideal treatment plan will depend on the individual’s symptoms, medical history, and lifestyle. Topical corticosteroids, topical calcineurin inhibitors, and antihistamines are commonly used to alleviate inflammation and itchiness. In some cases, phototherapy or oral immunosuppressants may be recommended.

Now that we’ve gained a deeper understanding of eczema and its causes, it’s important to remember that everyone’s experience with this condition is unique. Effective management involves finding a personalized approach that combines medical advice, self-care practices, and lifestyle modifications. In the next section, we’ll delve into the signs and symptoms of psoriasis, another chronic skin condition that affects many individuals worldwide.
Signs and Symptoms of Psoriasis
Psoriasis is a chronic skin condition that affects millions of individuals worldwide. It is characterized by distinctive symptoms that can vary in severity and presentation. By recognizing these signs, individuals can identify psoriasis early on and seek appropriate medical care. Here are some common symptoms of psoriasis:
- Redness: Psoriasis often causes patches of red and inflamed skin. These areas may appear as small, raised bumps or larger plaques.
- Scaling: One of the hallmark symptoms of psoriasis is the presence of silver or white scales on the skin’s surface. These scales can flake off and may be accompanied by itching or discomfort.
- Inflammation: Psoriatic lesions are typically accompanied by inflammation, causing the affected areas to feel warm to the touch. In severe cases, this inflammation can lead to joint pain and stiffness.
- Itching and Irritation: Psoriasis can cause intense itching and irritation, which can be both physically and emotionally distressing.
It’s important to note that psoriasis symptoms can vary from person to person and may even change over time. Some individuals may experience mild symptoms that come and go, while others may endure more persistent and severe manifestations. Understanding these symptoms is crucial for managing psoriasis effectively and seeking appropriate treatment options.
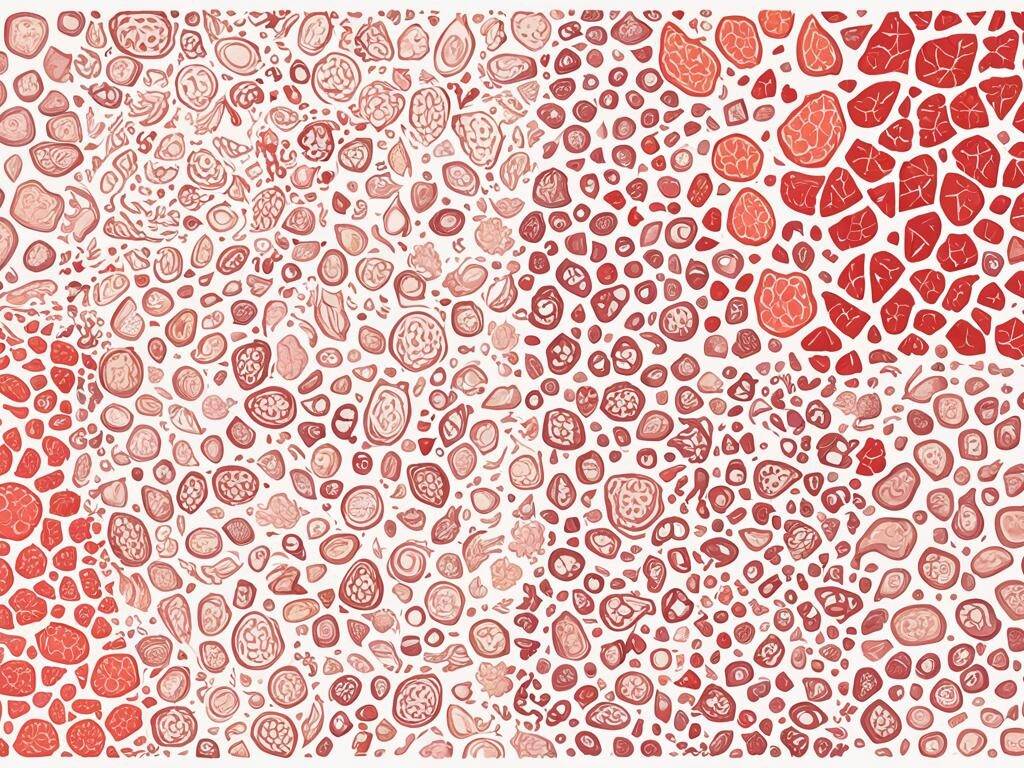
To visually depict the symptoms of psoriasis, refer to the image below:

“Psoriasis often causes patches of red and inflamed skin. It can be accompanied by silver or white scales, intense itching, and inflammation.”
Key Differences Between Eczema and Psoriasis
When it comes to skin conditions, eczema and psoriasis are often mistaken for one another due to their similar symptoms. However, it is important to understand the key differences between these two chronic skin conditions in order to receive appropriate treatment and management.
1. Appearance:
Eczema typically presents as red, itchy patches of skin that may ooze or crust over. The affected areas are often found on the face, hands, and inside the elbows and knees. In contrast, psoriasis is characterized by thick, silver-white scales on red, inflamed skin. Psoriasis lesions are most commonly found on the scalp, elbows, knees, and lower back.
2. Causes:
Eczema is believed to be caused by a combination of genetic and environmental factors. It is often triggered by allergens, irritants, and changes in temperature or humidity. On the other hand, psoriasis is thought to result from an overactive immune system and genetic predisposition. Certain factors, such as stress, infections, and medications, can also trigger psoriasis flare-ups.
3. Types:
There are several types of eczema, including atopic dermatitis, contact dermatitis, and dyshidrotic eczema. Each type has its own distinct characteristics and triggers. Psoriasis, on the other hand, can manifest in different forms, such as plaque psoriasis, guttate psoriasis, and pustular psoriasis. These different types affect various areas of the body and may require specific treatment approaches.
4. Treatment:
While both eczema and psoriasis are chronic conditions with no known cure, the treatment approaches differ. The primary goal of eczema treatment is to manage symptoms, reduce inflammation, and prevent flare-ups. This often involves the use of moisturizers, topical corticosteroids, and avoiding triggers. Psoriasis treatment focuses on controlling the rapid skin cell growth and managing inflammation. Treatment options include topical creams, oral medications, phototherapy, and biologic drugs.
5. Impact on Quality of Life:
Both eczema and psoriasis can significantly impact an individual’s quality of life. Eczema can cause intense itching, discomfort, and sleep disturbances. It may also affect self-esteem and social interactions. Psoriasis, with its visible skin lesions, can lead to embarrassment, self-consciousness, and depression. The psychological impact of these conditions should not be underestimated, and individuals should seek support from healthcare professionals and support groups.
Conclusion:
Understanding the differences between eczema and psoriasis is crucial for accurate diagnosis and effective management of these skin conditions. By recognizing the distinct characteristics, causes, and treatments, individuals can take proactive steps to address their specific condition and improve their overall well-being.

Effective Treatment for Eczema
When it comes to treating eczema, it’s essential to explore various options to find the most effective solution for managing symptoms and improving overall skin health. Here, we highlight some key treatment approaches and practical skincare tips to help individuals find relief from eczema.
1. Topical Creams and Ointments
One of the most common treatments for eczema is the application of topical creams and ointments. These medications help reduce inflammation, relieve itchiness, and restore moisture to the skin. Prescription creams containing corticosteroids or calcineurin inhibitors are often recommended for more severe cases, while over-the-counter moisturizers and hydrocortisone creams can provide relief for milder symptoms.
2. Lifestyle Changes
Aside from medication, making appropriate lifestyle changes can significantly impact eczema management. Maintaining a consistent skincare routine, avoiding harsh soaps and detergents, and opting for fragrance-free products can help minimize triggers and reduce flare-ups. Additionally, practicing good hygiene, such as moisturizing immediately after bathing and wearing breathable fabrics, can promote healthier skin.
3. Holistic Approaches
Besides traditional medical treatments, some individuals find relief from eczema symptoms through holistic approaches. These may include natural remedies, such as essential oils, herbal supplements, and dietary changes. However, it’s crucial to consult with a healthcare professional or dermatologist before trying any alternative treatments to ensure their safety and effectiveness.
4. Skincare Tips for Eczema Management
In addition to the treatments mentioned above, following these skincare tips can help individuals effectively manage their eczema:
- Keep your skin moisturized: Applying a good-quality moisturizer regularly can help soothe dryness and prevent eczema flare-ups. Look for products that are fragrance-free, hypoallergenic, and suitable for sensitive skin.
- Avoid hot showers or baths: Hot water can strip away the skin’s natural oils, leading to dryness and irritation. Opt for lukewarm water when bathing and limit showers to no more than 10 minutes.
- Use mild, non-irritating soaps: Choose gentle cleansers that are free from harsh chemicals and fragrances. Avoid scrubbing the skin vigorously and pat dry instead of rubbing with a towel.
- Manage stress: Stress can trigger eczema flare-ups, so it’s crucial to find effective stress-management techniques. Engage in activities that promote relaxation, such as meditation, yoga, or deep breathing exercises.
- Avoid known triggers: Identify and avoid specific triggers that worsen your eczema symptoms. These triggers may include certain foods, allergens, or environmental factors like extreme temperatures or humidity.
By combining these treatment options and incorporating practical skincare tips into daily routines, individuals can take control of their eczema and improve their quality of life. However, it’s essential to consult with a dermatologist to receive a personalized treatment plan and ongoing support.

What Causes Psoriasis?
Psoriasis is a chronic skin disorder that affects millions of people worldwide. It is essential to understand the underlying causes of this condition to develop effective treatment plans and strategies for prevention. Let’s explore the key factors that contribute to psoriasis:
- Genetics: Family history plays a significant role in psoriasis development. Having a close relative with psoriasis increases the likelihood of experiencing this condition. Studies have identified certain genetic variations associated with psoriasis, although the exact genetic mechanisms are still being researched.
- Immune system dysfunction: Psoriasis is considered an autoimmune disorder, where the immune system mistakenly activates an inflammatory response, leading to the rapid growth of skin cells. This abnormal immune system response causes the characteristic red, scaly patches associated with psoriasis.
- Environmental factors: External triggers can exacerbate psoriasis symptoms or even initiate flare-ups. Common environmental factors include cold weather, dry air, stress, infections, and certain medications. It is important to identify and manage these triggers to reduce the frequency and severity of psoriasis episodes.
To summarize, psoriasis is a complex condition influenced by both genetic and environmental factors, along with immune system dysfunction. By understanding these causes, individuals can work closely with healthcare professionals to develop personalized treatment plans that address their unique needs.
Quotes:
“Psoriasis is not just a skin condition; it is a chronic autoimmune disorder that requires comprehensive management.” – Dr. Jessica Cohen, Dermatology Specialist
Causes of Psoriasis
| Causes | Description |
|---|---|
| Genetics | Family history and certain genetic variations increase the risk of developing psoriasis. |
| Immune system dysfunction | Abnormal immune response triggers inflammation and excessive skin cell growth. |
| Environmental factors | Certain triggers such as cold weather, stress, and infections can worsen psoriasis symptoms. |

Treating Psoriasis Effectively
When it comes to managing psoriasis, it’s crucial to explore the various treatment options available. Successful treatment can help alleviate symptoms, reduce inflammation, and improve overall skin health. In this section, we will discuss some of the most effective treatments for psoriasis, including topical treatments, oral medications, and advanced therapies. By understanding the available options, individuals can work with their healthcare providers to develop a personalized treatment plan that suits their specific needs.
Topical Treatments
Topical treatments are often the first line of defense in psoriasis management. These medications are applied directly to the affected skin and can help soothe inflammation, reduce redness, and alleviate itching. Common topical treatments include:
- Corticosteroids: These anti-inflammatory medications help reduce redness, itching, and swelling.
- Vitamin D analogues: These synthetic forms of vitamin D slow down skin cell growth and reduce scaling.
- Topical retinoids: Retinoids normalize skin cell production and reduce inflammation.
- Calcineurin inhibitors: These medications help suppress the immune system response and reduce inflammation.
Oral Medications
In certain cases, topical treatments may not be sufficient to manage psoriasis symptoms. In such instances, oral medications may be prescribed by a healthcare provider. These medications work internally to target the underlying causes of psoriasis. Common oral medications for psoriasis include:
- Methotrexate: Methotrexate slows down the growth of skin cells and suppresses the immune system.
- Acitretin: Acitretin helps control skin cell growth and reduces inflammation.
- Cyclosporine: Cyclosporine suppresses the immune system response and reduces inflammation.
Advanced Therapies
For severe or resistant cases of psoriasis, advanced therapies may be recommended. These treatments are typically administered under the supervision of a healthcare professional. Advanced therapies for psoriasis include:
- Phototherapy: Phototherapy involves exposing the skin to ultraviolet light, which slows down skin cell growth and reduces inflammation.
- Biologics: Biologics are genetically engineered medications that target specific components of the immune system to reduce inflammation and inhibit skin cell growth.
| Treatment | Method of Administration | Benefits |
|---|---|---|
| Topical Treatments | Applied directly to the skin | Soothe inflammation, reduce redness, and alleviate itching |
| Oral Medications | Taken orally | Target underlying causes of psoriasis, reduce skin cell growth, and suppress immune system response |
| Advanced Therapies | Administered under medical supervision | Effective for severe or resistant cases, reduce inflammation, and inhibit skin cell growth |
The Burden of Chronic Skin Conditions
Eczema and psoriasis are two prevalent chronic skin conditions that significantly impact individuals’ physical and emotional well-being. Understanding the prevalence and impact of these skin diseases is crucial in addressing the challenges faced by those affected and promoting a supportive environment.
According to recent studies, approximately 31.6 million people in the United States alone have eczema, making it one of the most common skin diseases. Additionally, psoriasis affects approximately 8 million individuals in the country.
The burden of chronic skin conditions goes beyond physical discomfort and visible symptoms. These conditions can have profound effects on an individual’s self-esteem, mental health, and overall quality of life. The constant itchiness, pain, and skin irritation can lead to heightened stress, anxiety, and depression.
“Living with chronic skin conditions like eczema and psoriasis has its challenges. The constant battle with flare-ups and the impact on my self-confidence can be emotionally draining. It’s important that we raise awareness and support individuals in their journey towards self-acceptance and effective management.”
Raising awareness about the facts and realities of skin diseases like eczema and psoriasis is essential for combating stigmas and promoting empathy and understanding. By fostering an environment of support, individuals can feel empowered to seek proper medical care, share their experiences, and connect with others facing similar challenges.
Reducing the stigmas associated with these chronic skin conditions is a shared responsibility that requires education, compassion, and open dialogue. Together, we can create a society that embraces diversity, celebrates individuality, and supports the well-being of those affected by eczema and psoriasis.
The Prevalence of Eczema and Psoriasis in Numbers
| Condition | Prevalence (USA) |
|---|---|
| Eczema | 31.6 million |
| Psoriasis | 8 million |
Best Practices for Skin Care
Proper skin care is essential for individuals with eczema and psoriasis to alleviate symptoms and promote overall skin health. By following these dermatology insights and incorporating them into your daily routine, you can effectively manage and improve the condition of your skin.
1. Moisturize regularly
Key tip: Keeping your skin well-hydrated is crucial for managing eczema and psoriasis. Use moisturizers specifically formulated for sensitive skin, which are fragrance-free and do not contain harsh chemicals that can irritate your skin further. Apply moisturizer immediately after bathing or washing your face to seal in moisture.
2. Avoid triggers
Key tip: Identify and avoid triggers that can exacerbate your eczema or psoriasis. Common triggers include certain fabrics, harsh detergents, stress, and extreme weather conditions. Keep a journal to track any patterns or triggers that may cause flare-ups, enabling you to make informed decisions about your environment.
3. Use gentle skincare products
Key tip: Opt for skincare products specifically designed for sensitive skin. Look for gentle cleansers, hypoallergenic options, and fragrance-free products. Avoid using harsh soaps or exfoliants, as they can strip your skin of natural oils and increase irritation.
4. Protect your skin from the sun
Key tip: Shield your skin from harmful UV rays by wearing sunscreen with a high SPF, even on cloudy days. Choose a broad-spectrum sunscreen that provides protection against both UVA and UVB rays. Additionally, wear protective clothing, such as long-sleeved shirts and wide-brimmed hats, to minimize sun exposure.
5. Practice stress management
Key tip: High stress levels can trigger or worsen symptoms of eczema and psoriasis. Incorporate stress-reducing activities into your daily routine, such as yoga, meditation, or deep breathing exercises. Find activities that help you relax and unwind, as they can significantly impact the health of your skin.
Remember, everyone’s skin is unique, and what works for one person may not work for another. If you have any concerns or questions, it’s always best to consult with a dermatologist who can provide personalized recommendations based on your specific needs and condition.

6. Maintain a healthy lifestyle
| Healthy Lifestyle Habits | Description |
|---|---|
| Eat a balanced diet | Include nutrient-rich foods, such as fruits, vegetables, whole grains, and lean proteins, in your diet to support overall skin health. |
| Stay hydrated | Drink plenty of water to keep your skin hydrated from the inside out. |
| Get regular exercise | Engage in physical activity to improve circulation and promote healthy skin. |
| Get quality sleep | Ensure you are getting enough restful sleep, as lack of sleep can worsen skin conditions. |
By adopting these best practices for skin care, you can enhance your skin’s condition, manage symptoms of eczema and psoriasis, and improve your overall well-being. Remember to be patient and consistent in your routine, and always consult with a dermatologist for personalized advice.
Tips for Preventing Eczema and Psoriasis Flares
Preventing flare-ups and managing eczema and psoriasis requires a proactive approach and mindful lifestyle choices. By incorporating these practical tips into your daily routine, you can minimize the frequency and severity of symptoms associated with these chronic skin disorders.
1. Maintain a Consistent Skincare Routine
Establishing a regular skincare routine is essential for managing eczema and psoriasis. Use gentle, fragrance-free cleansers and moisturizers to keep your skin hydrated and protected. Apply moisturizer immediately after showering to lock in moisture.
2. Avoid Triggers and Irritants
Identify and avoid common triggers that can worsen eczema and psoriasis symptoms. These may include harsh soaps, certain fabrics, pet dander, and environmental allergens. Wear soft, breathable clothing and opt for fragrance-free, hypoallergenic products.
3. Manage Stress Levels
Stress can exacerbate eczema and psoriasis flares. Practice stress management techniques, such as deep breathing exercises, meditation, and regular physical activity. Engaging in activities you enjoy can also help reduce stress levels and promote overall well-being.
4. Follow a Healthy Diet
Eating a balanced diet rich in fruits, vegetables, lean proteins, and omega-3 fatty acids can support skin health and reduce inflammation. Limit your intake of processed foods, sugar, and alcohol, as they can trigger flare-ups.
5. Keep Your Skin Moisturized
Apply moisturizer multiple times throughout the day, especially on areas prone to dryness and irritation. Look for moisturizers that contain ceramides or hyaluronic acid, as they help restore and lock in moisture.
6. Protect Your Skin from Sun Exposure
UV rays can trigger flare-ups and worsen symptoms of eczema and psoriasis. Protect your skin by wearing broad-spectrum sunscreen with an SPF of 30 or higher, and seek shade during peak hours of sun exposure.
7. Seek Professional Guidance
If your eczema or psoriasis symptoms persist or worsen despite your efforts, consult a dermatologist. They can provide customized treatment plans and offer additional guidance on managing your condition.

8. Connect with Supportive Communities
Joining support groups or online communities can provide a valuable source of emotional support, advice, and shared experiences. Connecting with others who understand the challenges of living with eczema and psoriasis can help you feel less alone in your journey.
| Tips for Preventing Eczema and Psoriasis Flares | Description |
|---|---|
| Maintain a Consistent Skincare Routine | Establish a regular skincare routine using gentle, fragrance-free products. |
| Avoid Triggers and Irritants | Identify and avoid common triggers that can worsen symptoms. |
| Manage Stress Levels | Practice stress management techniques to reduce flare-ups. |
| Follow a Healthy Diet | Eat a balanced diet to support skin health and reduce inflammation. |
| Keep Your Skin Moisturized | Apply moisturizer multiple times a day to hydrate your skin. |
| Protect Your Skin from Sun Exposure | Wear sunscreen and seek shade to prevent UV-triggered flare-ups. |
| Seek Professional Guidance | Consult a dermatologist for personalized treatment plans. |
| Connect with Supportive Communities | Join support groups for emotional support and shared experiences. |
Coping with Emotional Challenges
Living with skin conditions like eczema and psoriasis can take a toll on one’s emotional well-being. The visible symptoms, such as redness, flaking, and itching, can lead to self-esteem issues and feelings of embarrassment. Additionally, the impact of these conditions on daily life, from managing flare-ups to finding effective treatments, can cause anxiety and emotional distress.
It’s important to acknowledge and address the emotional challenges that can arise from living with eczema and psoriasis. By understanding your emotions and actively seeking support, you can develop effective coping mechanisms to navigate these challenges and improve your overall well-being.
“Living with a chronic skin condition like psoriasis or eczema requires resilience and self-compassion. It’s important to remember that you are not alone in this journey and that support is available. Reach out to friends, family, or support groups who can provide understanding and empathy.”
Building a strong support system is crucial when coping with the emotional aspects of eczema and psoriasis. Surround yourself with loved ones who are supportive and understanding, and consider joining local or online support groups where you can connect with others who share similar experiences.
Self-Care for Emotional Well-being
Practicing self-care plays a vital role in managing the emotional impact of eczema and psoriasis. Here are some self-care strategies to consider:
- Practice relaxation techniques: Engage in activities like deep breathing exercises, meditation, or yoga to reduce stress and promote a sense of calm.
- Pursue hobbies: Find activities or hobbies that bring you joy and help distract from negative thoughts or stressors.
- Set realistic goals: Break down tasks into manageable steps and celebrate your achievements, no matter how small they may seem.
- Take care of your overall health: Maintain a healthy lifestyle by eating nutritious meals, exercising regularly, and getting enough sleep.
Remember, seeking professional help is just as important as self-care. If you find that your emotional well-being is severely impacted by eczema or psoriasis, consider consulting with a mental health professional who can offer guidance and support tailored to your needs.
Inspirational Quotes
“Having eczema or psoriasis doesn’t define who you are. Your strength and resilience in facing these challenges do.”
“Self-acceptance and self-love are powerful tools in overcoming the emotional challenges that come with chronic skin conditions like eczema and psoriasis.”
Remember that you are more than your skin condition. Focus on nurturing your emotional well-being, seeking support, and practicing self-care. With the right mindset and coping strategies, you can navigate through the emotional challenges of living with eczema and psoriasis.

Advancements in Dermatological Treatments
In the field of dermatology, ongoing research and technological advancements have paved the way for innovative treatments and therapies for chronic skin disorders such as eczema and psoriasis. These developments offer hope to individuals seeking effective management strategies and improved quality of life.
Molecular Targeted Therapies
One of the significant breakthroughs in dermatology is the emergence of molecular targeted therapies. These treatments specifically target the underlying mechanisms and pathways involved in chronic skin disorders, providing more precise and effective outcomes. By focusing on key molecules and receptors, these therapies offer targeted relief for symptoms and help manage the long-term progression of eczema and psoriasis.
Biologics
Another notable advancement in dermatological treatments is the increasing use of biologics. These medications are derived from living organisms and act on specific components of the immune system responsible for chronic inflammation in the skin. Biologics offer a targeted approach to managing eczema and psoriasis by interrupting the inflammatory process and reducing symptoms such as itching, redness, and scaling.
“Biologics have revolutionized the treatment of chronic skin disorders by offering a new level of precision and effectiveness.” – Dr. Emily Thompson, Dermatologist
Phototherapy
Phototherapy, also known as light therapy, has been a longstanding treatment modality for eczema and psoriasis. However, recent advancements have allowed for more targeted and controlled delivery of light, maximizing therapeutic benefits while minimizing potential side effects. Narrowband UVB therapy and excimer laser therapy are examples of these enhanced phototherapy techniques that provide localized treatment and improved outcomes.
Advanced Topical Formulations
The formulation of topical treatments has evolved significantly in recent years. Dermatologists now have access to novel delivery systems that enhance the penetration and efficacy of active ingredients. These advancements include encapsulated technologies, nanoemulsions, and liposomal formulations, allowing for better drug delivery to the affected areas and improved symptom relief.
Comparative Overview of Advancements in Dermatological Treatments
| Treatment | Advantages | Disadvantages |
|---|---|---|
| Molecular Targeted Therapies | – Precise targeting of key molecules – Effective management of underlying mechanisms – Reduced systemic side effects |
– Costly – Limited long-term safety data |
| Biologics | – Targeted approach to inflammation – Significant symptom relief – Better long-term disease control |
– High cost – Risk of infections |
| Phototherapy | – Non-invasive treatment option – Controlled and targeted delivery of light – Suitable for widespread symptoms |
– Potential risk of skin damage – Regular treatment visits required |
| Advanced Topical Formulations | – Enhanced drug delivery to affected areas – Improved symptom relief – More convenient and user-friendly |
– Possible skin irritation – Variability in individual response |
These advancements in dermatological treatments hold great promise for individuals with eczema and psoriasis. They offer new avenues for effectively managing symptoms, improving quality of life, and potentially achieving long-term remission. Consulting with a dermatologist is essential to understanding the most suitable treatment options based on individual needs, medical history, and severity of the condition.
Essential Tips for Living with Eczema and Psoriasis
After exploring eczema and psoriasis in-depth, it’s time to equip you with essential tips to manage these chronic skin conditions effectively. By incorporating these recommendations into your daily routine, you can improve your quality of life and minimize the impact of eczema and psoriasis.
Eczema Skincare Tips:
- Moisturize regularly: Apply a fragrance-free moisturizer to keep your skin hydrated and prevent dryness, a common trigger for eczema.
- Avoid irritants: Use gentle, hypoallergenic skincare products, and avoid harsh soaps, detergents, and other potential irritants.
- Identify triggers: Keep a journal to track potential triggers like certain foods, stress, or environmental factors. Once identified, take steps to avoid or minimize exposure to these triggers.
- Protect your skin: Wear protective clothing, such as cotton gloves and long sleeves, to shield your skin from potential irritants and allergens.
Psoriasis Skincare Tips:
- Manage stress: Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises, as stress can exacerbate psoriasis symptoms.
- Moisturize regularly: Apply a moisturizer to your skin immediately after bathing to lock in moisture and relieve dryness.
- Sun protection: Shield your skin from excessive sun exposure by using sunscreen with a high SPF and wearing protective clothing, as sunlight can trigger psoriasis flare-ups.
- Avoid hot baths/showers: Opt for lukewarm water instead of hot water, as hot water can dry out your skin and worsen psoriasis symptoms.
“Managing eczema and psoriasis requires a comprehensive approach, involving skincare, lifestyle changes, and proactive measures to minimize triggers.”
Remember, it’s essential to consult a dermatologist for personalized treatment plans and expert guidance. With the right strategies in place, you can lead a fulfilling life and effectively manage your eczema or psoriasis.
| Eczema Skincare Tips | Psoriasis Skincare Tips |
|---|---|
| Moisturize regularly | Manage stress |
| Avoid irritants | Moisturize regularly |
| Identify triggers | Sun protection |
| Protect your skin | Avoid hot baths/showers |
When to Consult a Dermatologist
When it comes to managing eczema and psoriasis, seeking professional guidance from a dermatologist is crucial. Dermatologists specialize in diagnosing and treating various skin conditions, including eczema and psoriasis. Their expertise and experience can provide individuals with personalized treatment plans, ensuring the most effective management of their symptoms.
If you are experiencing persistent or worsening symptoms of eczema or psoriasis, it may be time to consult a dermatologist. Here are some guidelines and indicators that suggest seeking professional care:
- Severe Symptoms: If your eczema or psoriasis symptoms are severe, such as intense itching, widespread rash, or significant pain, it is important to consult a dermatologist for prompt evaluation and treatment.
- No Improvement: If your symptoms have not improved with over-the-counter treatments or self-care measures, a dermatologist can assess your condition, provide a more accurate diagnosis, and recommend more effective treatment options.
- Chronic Condition: If you have been diagnosed with eczema or psoriasis and are struggling to manage your condition on your own, a dermatologist can offer expert guidance on long-term management strategies and help you achieve better control over your symptoms.
- Unsure Diagnosis: If you are unsure about the nature of your skin condition or suspect it may be eczema or psoriasis, a dermatologist can conduct a thorough examination, perform diagnostic tests if necessary, and provide an accurate diagnosis.
- Extra Support: Even if you have been managing your eczema or psoriasis successfully, consulting a dermatologist periodically can offer additional support, advice, and updated treatment options to keep your condition under control.
Remember, each individual’s situation is unique, and a dermatologist can customize a treatment plan that best suits your specific needs. Don’t hesitate to reach out to a dermatologist if you have any concerns or questions about managing your eczema or psoriasis.
Expert Tip:
If you’re unsure whether to consult a dermatologist, it’s always better to err on the side of caution. Seeking professional advice can help you better understand your condition and explore the most effective treatment options available.
By partnering with a dermatologist, you can ensure that you receive comprehensive care, expert guidance, and effective treatment for managing your eczema or psoriasis. Take the first step towards healthier skin by scheduling an appointment with a dermatologist who specializes in dermatology today.
Conclusion
Understanding eczema and psoriasis is essential for individuals seeking effective management strategies for these chronic skin conditions. Throughout this article, we have explored the causes, symptoms, and treatment options for both eczema and psoriasis.
By highlighting the key differences between these two skin conditions, we have provided valuable insights that can inform personalized treatment plans. Whether it’s managing triggers, seeking appropriate medical attention, or adopting proper skincare practices, individuals can make informed decisions in their journey towards healthier skin.
It is important to remember that while living with eczema and psoriasis can present challenges, individuals can still lead fulfilling lives with the right support and management strategies. By practicing self-care, seeking professional guidance from dermatologists, and staying up-to-date on advancements in treatment options, individuals can find relief and maintain optimal skin health.
In conclusion, understanding eczema and psoriasis empowers individuals to take control of their skin health. By being informed and proactive, individuals can manage their symptoms, reduce flare-ups, and enjoy a higher quality of life despite these chronic skin conditions.

